Varicose veins of the lower extremities are a problem that affects more than 60% of the world's population. The term "varicose veins" from Latin "varx" is interpreted as "expansion". Hence, the definition of a pathological condition is an enlargement of the lumen of the vessels of the lower extremities and pelvic organs, which significantly worsens the blood flow in the vessels and therefore worsens the general condition of the patient. In the following material we will consider the causes of varicose veins, possible complications of the disease and the main ways to deal with the pathology.
Causes and risk factors: everyone is sensitive to it
Important:If varicose veins outnumber young people under the age of 25, the sex ratio is 50: 50. That is, both boys and girls are equally ill. In older adults, women are more likely to have varicose veins due to significant age-related changes in pregnancy and hormonal levels.
If we think of varicose veins from the inside, anatomically, the expansion of the lumen of the veins occurs due to a malfunction of the venous valves that regulate blood flow. Defective valves do not close completely with every heartbeat. As a result, the blood coming from the heart with concussions moves to the lower extremities due to gravity.
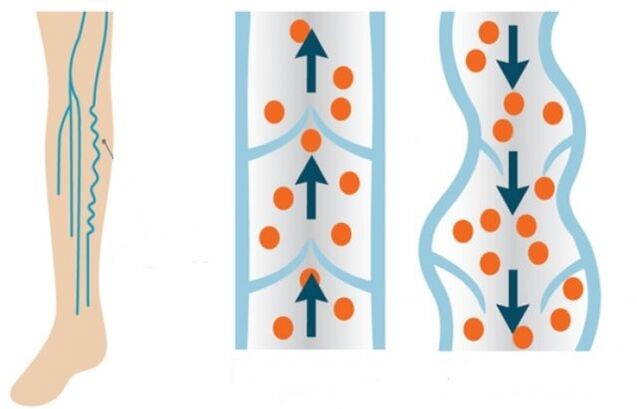
Normally, the valves should close and allow blood to flow to the legs in parts. Unfortunately, blood flow enters the legs more intensively and moves less intensively in the opposite direction due to the same poor functioning of the valve system. The blood vessels in the blood-filled legs lose their elasticity and stretch over time.
The main predisposing factors for the development of pathological conditions of blood vessels are:
- genetic component (the disease can be transmitted through the female or male line within the family);
- overweight;
- delayed pregnancy;
- passive lifestyle;
- excessive physical activity;
- smoking and drinking alcohol;
- hormonal disorders.
Men's problems
Given the causes of varicose veins, depending on the sex of the patient, they are slightly different in men and women. Rather, each of the different sexes is prone to certain habits, which can sooner or later lead to vascular pathology of the lower extremities. Thus, the risk factors for men are:
- strength training by lifting weights from a squat position;
- overweight and obesity;
- an unbalanced diet that often causes constipation;
- pathological processes of the kidneys (tumors of various etiologies);
- groin hernia;
- sedentary work;
- to smoke and drink alcohol.
Important:Men are characterized not only by the development of varicose veins of the lower extremities, but also by varicose veins of the spermatic cord. This pathology is called varicocele. Such a situation remains hereditary, ie it is only genetic and cannot be prevented even with advanced preventive measures. Only 2-4% of men suffer from varicocele. The cause of the pathology is the asymmetrical anatomical location and structure of the male genitals.
Varicose veins are more difficult for men than women because they suffer from false restraint or do not have time to consult a specialist at the beginning of the disease.
Women's varicose veins have their own laws
Varicose veins are more "familiar" in women than men. More than 80% of women suffer from vascular pathology of the legs. In addition, the risk group includes members of the fair sex who choose this lifestyle or live in the following conditions:
- wear narrow heels;
- sitting or standing work;
- hereditary predisposition;
- changes in hormonal levels during pregnancy or with autoimmune diseases;
- wear very tight underwear, jeans;
- to smoke;
- small amounts of fruits and vegetables in the diet (regular diets and starvation);
- love of tanning (frequent visits to the solarium or staying in direct sunlight);
- acute weight loss;
- low mobility.
Pregnancy is "the place where a dog is buried"
Although the causes and treatment of varicose veins, which should be prescribed and prescribed only by a phlebologist, are not initially observed in a woman, they are found in 30% of cases during pregnancy. The main trap here is in the growing fetus and at the same time in the uterus, which tightly compresses the pelvic organs. As a result, blood circulation in the lower part of the body is significantly impaired. It is difficult for blood to flow back upwards from the legs. This effect on the deep veins of the legs causes the veins to actively stretch in both width and length.
In addition to uterine enlargement and pressure on the vessels of the pelvic organs, varicose veins in pregnant women also develop under the influence of the following factors:
- Increased blood clotting. Thus, nature insures a woman against major blood loss during childbirth. Thicker blood moves more through the arteries.
- An increase in the level of the hormone progesterone leads to relaxation of the muscles and blood vessels of the uterus, which allows the fetus to grow freely and without tone as it grows. But at the same time, the walls of the remaining arteries relax. The arteries become less elastic and the thick blood stretches the walls, which are weakened by the effects of progesterone.
- An increase in blood pressure for a better oxygen supply to the fetus. As a result, the body tries to pump thick blood from comfortable vessels quickly. The volume in the legs therefore increases.
- Low mobility of a pregnant woman with abdominal enlargement. This causes blood stasis in the legs and pelvic organs.
Complications of varicose veins
If varicose veins are not treated and cared for, over time the patient may develop very serious complications that may require a full-fledged surgical intervention. In the worst case, the patient may undergo amputation of the affected joint. Below we will review the most common and dangerous complications of varicose veins.
Chronic venous insufficiency
With the development of such a complication there is an active failure of venous valves. In addition, the pathological process is divided into four stages:
- Zero. The patient feels a small swelling and rarely pain in the legs after a hard day.
- First. The venous network of dilated vessels is visible on the surface of the skin.
- The second. Blood clots and swollen veins with nodules inside are clearly visible. There is redness of the skin in areas with inflamed veins, itching, wounds.
- Third. Trophic ulcers form in the legs with inflamed veins.
Important:Symptoms of chronic venous insufficiency are itching of the legs, pain, burning sensation during prolonged sitting, swelling, night cramps.
Superficial vascular thrombophlebitis
In this case, the patient develops a blood clot. Coagulation actively closes the lumen of blood vessels and complicates blood flow. In most cases, clots and clots are localized in the veins in the lower third of the thigh or in the upper third of the leg. Symptoms of venous thrombophlebitis:
- redness of the skin of the legs where coagulation occurs;
- pain in the legs;
- during palpation - induration in the vessels.
Important:With thrombophlebitis, you need to wear compression stockings. The compression formula should be chosen by a specialist - angiosurgeon or phlebologist.
Trophic ulcer
This complication already manifests itself in the later stages of venous insufficiency. First, the patient develops increased vascular permeability. A whitish seal with a lacquer-like surface is formed on the surface of the skin. An ulcer forms under it. At the slightest damage to the inflamed area, the ulcer opens and the exudate begins to separate. The leaking wound can become infected with the latter, which leads to purulent inflammatory processes.
Important:In this case, complete healing of the wound is required first, followed by full surgical intervention to remove the affected vessels.
Pulmonary embolism
An equally dangerous complication is when the thrombus separates from the inflamed vein and moves to the pulmonary artery. This artery is involved in the organization of blood flow in a small circle that directly affects the right ventricle of the heart. If the diameter of the separated thrombus is less than the lumen of the artery, the clot moves to the branches of the pulmonary artery and provokes pulmonary edema or infarction. In this case, the patient will feel significant chest pain. A wet cough mixed with blood, an increase in body temperature and weakness will also appear. If the diameter of the clot is equal to the diameter of the lumen of the pulmonary artery, the patient has a sudden blockage and death.
Separation of a blood clot can occur as a result of the following conditions:
- performing surgical interventions;
- oncology;
- heart problem;
- long bed rest.
Conservative and surgical treatment
Varicose veins can be treated both conservatively and surgically, depending on the pathological stage and the patient's condition. Phlebotonic drugs are indicated with conservative treatment. Externally, gels and venotonic ointments based on horse chestnut are used. It should be understood that conservative treatment works only in the early stages of varicose veins.
Additional measures in the conservative treatment of varicose veins include physical activity (walking) and wearing compression stockings.
Minimally invasive and surgical treatment methods
If the process of varicose veins and venous insufficiency is long overdue, they resort to minimally invasive or full-fledged surgery to improve the patient's condition. Minimally invasive intervention methods include:
- Sclerotherapy. In this case, a special sclerosis drug is injected into the lumen of the patient's varicose vein using a thin insulin needle. The injected substance first causes inflammation and then the patient develops vascular sclerosis. The lumen of the diseased vessel simply grows. The technique has a more cosmetic effect, but does not solve the problem (cause) of the pathology. Relapse is possible after sclerotherapy. Contraindications to such an intervention are pregnancy, lactation and intolerance to the components of the drug.
- Don't peel. Using this method, the patient's vein is removed using the thinnest probe. The peculiarity of the surgical intervention is that it is possible to remove the diseased part of the vessel, leaving only the healthy parts. The operation is performed through two endoscopic perforations located on either side of the inflamed vascular area. That is, after such an intervention, scars and scars will not be visible.
- Microflebectomy. Removal of the diseased vessel is performed through several small incisions in the skin.
- Laser coagulation. Laser exposure to the lumen of a diseased vessel. As a result, the vascular lumen is completely enlarged.
Full-fledged surgery (abdominal surgery) is called phlebectomy. In this method, the surgeon makes a complete incision in the skin of the foot to remove the entire superficial vein. Indications for such an operation:
- large varicose veins;
- large lumen of the diseased vessels (more than 10 mm);
- thrombophlebitis;
- presence of large varicose veins;
- formation of trophic ulcers in the patient;
- lack of effectiveness of minimally invasive surgery.
Traditional methods of treatment
In the early stages of the pathology, you can resort to folk remedies to treat varicose veins. In particular, you can use the following folk remedies in combination with medication:
- Tomatoes are green. Thin slices of vegetables are placed in the area of inflamed veins and fixed with a bandage. You should change such applications every 2-3 hours. The course of treatment is until the condition clearly improves.
- Potato. The dressing soaked in freshly squeezed potato juice is applied to the feet. Cover with cling film. Such applications are best done at night until the patient's condition improves.
- Apple cider vinegar. Preferably homemade. Vinegar is diluted in water (1 cup water and 2-3 tablespoons of vinegar). A bandage is moistened in a solution and applied to the area of the diseased veins. The dressing is adjusted at night. At night, you can simply lubricate your feet with this solution. It is shown that it contains vinegar. To avoid burning the esophagus with vinegar, add 1 tablespoon of apple cider vinegar and a teaspoon of honey to a glass of water (esophageal walls are very sensitive to acids). The mixture is for starvation in the morning. The duration of treatment with vinegar is 30 days.
- The horse was chestnut. Plant flowers in the amount of 50 grams. Pour 0, 5 liters of alcohol and insist two weeks in a dark place, shaking the mixture periodically. The finished product is filtered through a mesh and drink three times a day, one tablespoon at a time. The mixture is washed with water. The course of treatment is 7 days. Then a 14-day break and again a seven-day course. Treatment according to this scheme is carried out until the end of the infusion. It can then be retrained and the therapy regimen repeated.
- Burdock. In this case, fresh leaves of the plant are used to eliminate the disease. At night, sore feet are rubbed with Vishnevsky's ointment and wrapped with burdock leaves. Everyone is straightened with a bandage and put on compression stockings. The bandage is worn for three days, then removed and everything is washed. It is possible to treat in this way throughout the summer, growing fresh burdock.
Important:Such treatment is contraindicated in patients with high acidity of gastric juice.

results
It is worth noting that varicose veins are often an irreversible pathology. Therefore, it is very important to pay attention to the health of your feet. Especially if you have a genetic predisposition to varicose veins. It is enough to give up bad habits, balance your daily diet, walk more and drink enough clean water a day. At the slightest sign of varicose veins, it is advisable to contact an authorized phlebologist immediately to prevent complications of the disease. Remember, your health and the internal health of your feet are entirely yours. And modern medicine and the hands of a specialist can work wonders.























